As real-world data and advanced analytics start to transform life sciences, Medical Affairs is transitioning to a new strategic role. However, grasping this opportunity requires a significant mindset shift, and MA professionals will need to acquire a new skillset.
 The amount of data we are currently generating is astronomical. According to one often-quoted article on Forbes.com, some 90 percent of the data in the world was generated over the past two years alone. [1]
The amount of data we are currently generating is astronomical. According to one often-quoted article on Forbes.com, some 90 percent of the data in the world was generated over the past two years alone. [1]
Today’s world is defined by data, with 2.5 quintillion bytes of data created everyday – and that pace is only accelerating as the Internet of Things (IoT) expands. No surprise then that Mike Devoy, Chief Medical Officer, Head of Medical Affairs & Pharmacovigilance at Bayer, predicts that the time is right for digital to transform our thinking about healthcare.
“I believe digital is going to become more and more important and, over time, it will transform how healthcare is delivered and also how drugs are researched and discovered. We’ve seen the explosion in data coming from the intensified use of wearable devices, sensors and so on, but now we have the computer power and the technology to start to really understand that information and turn it into relevant action.”
Moreover, Medical Affairs stands at the very epicenter of this digital revolution in healthcare, given the function’s scientific credentials and its potential to define, gather and interpret data to generate the insights that will deliver meaningful outcomes for the entire spectrum of healthcare stakeholders – but especially patients and healthcare professionals.
 “In Medical Affairs, we have a unique role because we have a deep understanding of our products and knowledge of diseases. We should be looking to fit the new knowledge and insights that we can collect from Real-World Evidence (RWE) into delivering even better solutions for patients and the healthcare system. And, because we are in daily contact with healthcare professionals, patient associations and other stakeholders, we should be the ones who play a critical role in transforming that into something that actually meets the needs and provides services and solutions for end-users. By connecting what’s coming out of our R&D, the strategy behind the products from a commercial point of view, we could build this into an overall, integrated patient care vision.”
“In Medical Affairs, we have a unique role because we have a deep understanding of our products and knowledge of diseases. We should be looking to fit the new knowledge and insights that we can collect from Real-World Evidence (RWE) into delivering even better solutions for patients and the healthcare system. And, because we are in daily contact with healthcare professionals, patient associations and other stakeholders, we should be the ones who play a critical role in transforming that into something that actually meets the needs and provides services and solutions for end-users. By connecting what’s coming out of our R&D, the strategy behind the products from a commercial point of view, we could build this into an overall, integrated patient care vision.”
Top three areas of focus
 Dr Devoy sees scope for applying digital innovation across a range of areas but suggests that R&D, patient outcomes, and safety are the three to focus on initially. There is significant potential for how we conduct clinical trials: for example, using artificial intelligence (AI) within R&D as part of the drug discovery process, and also helping to better characterize and stratify disease and the according patient populations for study.
Dr Devoy sees scope for applying digital innovation across a range of areas but suggests that R&D, patient outcomes, and safety are the three to focus on initially. There is significant potential for how we conduct clinical trials: for example, using artificial intelligence (AI) within R&D as part of the drug discovery process, and also helping to better characterize and stratify disease and the according patient populations for study.
“If you look at a disease such as heart failure, we still have a pretty simple way of categorizing patients based on clinical examination, imaging investigation and some clinical tests. But almost certainly there are more different types of heart failure in terms of the underlying pathophysiology. So, if we can apply digital learning and artificial intelligence to better stratify these areas and therefore to personalize treatments, then I think we will overcome a lot of hurdles to improving patient care.”
Cost is already a major issue in healthcare and digital has the potential to help unlock cost-savings for healthcare systems and wider society, as well as for industry.
Digitally integrating electronic medical records (EMR), both to identify patients and then also to follow up and stay connected with them is another considerable area of potential.
“I think there are already examples starting to happen that could dramatically reduce the cost of particularly large outcome studies which you have to do in areas like cardiovascular. There are significant gains that can be achieved by applying technology to make the studies more efficient, more precise, simpler to conduct, and so able to be conducted more quickly and more cheaply.”
Digitally integrating electronic medical records (EMR), both to identify patients and then also to follow up and stay connected with them is another considerable area of potential. “We should be looking at diagnostic technology and EMR to detect and diagnose disease much earlier and enable informed decision-making – that will allow us to intervene with prevention before people become physically sick at the stage they might currently be diagnosed.”
Adherence and product safety are two further areas of great promise for digital.
“For as long as I’ve been in the industry, something we’ve talked about but struggled with is finding ways that we can help patients adhere to the treatment that they’ve been prescribed, so that we actually deliver better outcomes. The use of sensors, wearables and other applications may offer such a solution for enhancing treatment adherence. I also believe that we can help better understand the benefit-risk of our products using AI and big data approaches to identify safety signals and issues with products earlier.”
Challenges
However, the fact that the technology is so new and accompanied by such a weight of expectation inevitably implies some formidable challenges.
 “We read every day about how digital is transforming everything we do – be that personal finance, or interactions with retail – so I think the expectation from society is that healthcare will also transform in that way. But, clearly, healthcare has quite rightly some additional challenges relating to the sensitivity of people’s health data and taking the right care of that. So, we need to work with regulators, governments, patients and physicians to make sure that these solutions are accessible, trusted, compliant and fitted to people’s expectations.
“We read every day about how digital is transforming everything we do – be that personal finance, or interactions with retail – so I think the expectation from society is that healthcare will also transform in that way. But, clearly, healthcare has quite rightly some additional challenges relating to the sensitivity of people’s health data and taking the right care of that. So, we need to work with regulators, governments, patients and physicians to make sure that these solutions are accessible, trusted, compliant and fitted to people’s expectations.
As companies, we need to adapt to working and developing and being successful in a digital environment. So, that will mean hiring and developing new talent with the right skills in areas like data science and data privacy. But, also, we are not just competing with other healthcare companies, now, but numerous other technology companies and other industries for those skill sets. It’s not just hiring new people, but also developing capabilities, making our current employees more savvy about working with digital – how those technologies could be applied, what the potential options are.
One area where Medical Affairs in most companies is usually taking a lead is understanding, communicating and generating real-world evidence. That is going to put increasing demands on Medical Affairs organizations to be able to access and analyze large data sets. To turn this into useful and meaningful evidence that can inform both the decisions of our organizations but also inform other stakeholders such as regulators, physicians and patients.”
New digital culture
At Bayer, digital is already driving new business models and the organization is cultivating a new digital culture across its various businesses. “Digital will change our business models and how we relate to patients and healthcare professionals – it’s a high priority for us and we have created a strategic framework as well as a digital agenda to help us become future-ready. We really want to make digital technologies an integral part of our overall business acumen, value chain, lifecycle management and decision-making, and we’re looking at that as a critical aspect of our overall business. We also recognise that a lot of the innovation and expertise is going to come from outside and from different areas, from different sorts of companies.
 “One thing I believe we’ve done very successfully is build up an approach for actively seeking external collaboration. ”Among the initiatives is a global program called Grants4Apps, established in 2013, where Bayer reaches out to companies that are in the early stages of developing in the digital health and care space. Bayer acts as incubator and offers mentoring support and access to Bayer expertise and knowledge to help them develop their business models and solutions. Meanwhile, the Grants4Apps Dealmaker program is a unique opportunity to acquire Bayer as a customer and is tailored for mature teams, startups and companies that have a solution ready to go for identified challenges.
“One thing I believe we’ve done very successfully is build up an approach for actively seeking external collaboration. ”Among the initiatives is a global program called Grants4Apps, established in 2013, where Bayer reaches out to companies that are in the early stages of developing in the digital health and care space. Bayer acts as incubator and offers mentoring support and access to Bayer expertise and knowledge to help them develop their business models and solutions. Meanwhile, the Grants4Apps Dealmaker program is a unique opportunity to acquire Bayer as a customer and is tailored for mature teams, startups and companies that have a solution ready to go for identified challenges.
We also partner with research institutions across the world and, where it makes sense, with various technology companies that are also entering the healthcare space. You look at who are the partners that are meaningful to your stakeholders – like patients and healthcare professionals – and how do you do something with that partner that creates more value. We strive to enhance our ecosystem (for example with subsidiaries in San Francisco and Boston) and constantly monitor the external environment trying to link business challenges and evidence needs to potential technological solutions.”
Quality and quantity of data
Nevertheless, to harness the potential of RWE – both from EMR and sensors and devices – companies such as Bayer will need to make sure they have the ability to handle large volumes of data, that the data is of the right quality and data privacy is respected, and that they have the right skills and methodological approach to succeed in this space. “I think we need to make sure that we operate to a high standard of scientific integrity and quality because there are certainly risks if you don’t. And you need to bring in different skill sets in areas that will allow you to collect, analyse and interpret that data.” Bayer has been working hard to find people with skills in areas of big data analysis, including data scientists and epidemiologists.
Strategic role
In conclusion, Dr Devoy emphasizes that all of these changes imply a significant mindset shift on the part of MA professionals, who will be moving from their traditional support role to much more of a strategic focus. This will involve the function engaging much earlier in the value chain.
“Medical Affairs will get involved in the early project discussions [helping] research colleagues think about the best approach in terms of patient target groups, disease, models, linking to external expertise and knowledge. He also envisages Medical building a strategy aligned with global and key countries where the function will conceive or build a medical strategy aligned with the overall plan, both in terms of data generation and communication.
“In some key topics, such as real-world evidence, Medical is very much the function that takes the lead role in working with all the internal and external stakeholders to create the strategy and then execute it across the organization. You see it in very tangible things in terms of resource deployment, which has changed very significantly over the last five years.”
Going forward, Dr Devoy sees Medical as being the trusted partner between businesses and key external stakeholders – patient bodies, physicians and regulators – articulating the value companies are providing to healthcare systems and to patients. MA potentially has a unique understanding of how that value can be created and delivered, and a key role in developing the evidence and solutions around that value in collaboration with internal and external partners such as R&D colleagues, digital providers, physician groups and patient advocates.
“As patients become more empowered to make healthcare choices, it’s more important than ever for healthcare companies to create compelling and satisfying experiences. Digital solutions and innovation have never been more at the forefront of healthcare and are an important part of Bayer’s long-term strategy. These solutions can drive down costs or boost efficiency, build connections to patients and dramatically improve patient outcomes.”
About
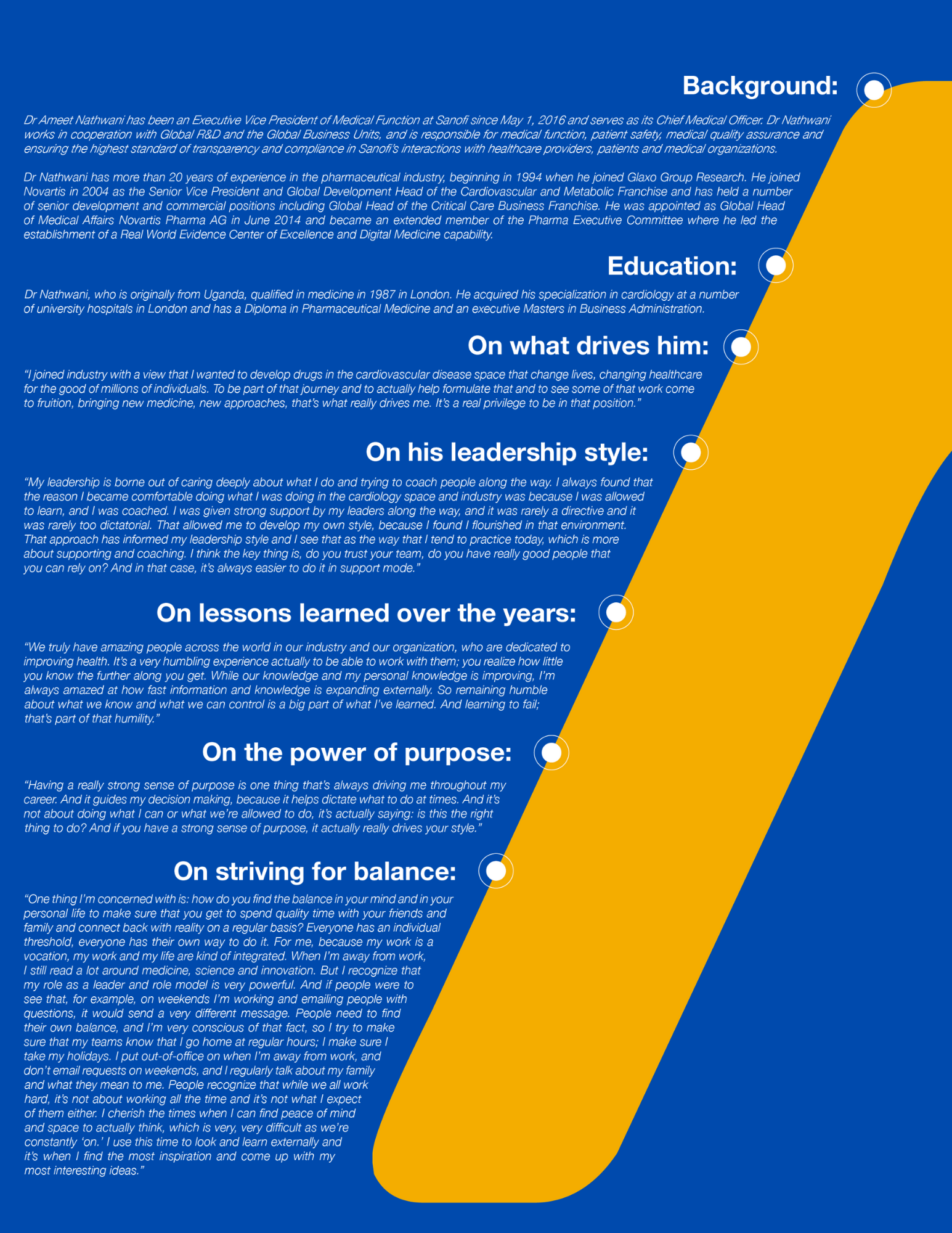
Dr Michael Devoy is the Executive Vice President for Medical Affairs and Pharmacovigilance for the Pharmaceuticals Division at Bayer AG. He is also the Chief Medical Officer of Bayer AG. He joined the former Schering AG in 2005 as Senior Vice President of Global Medical Development and was appointed to his current position in 2014.
Dr Devoy studied Medicine and Pharmacology at University College London and graduated with a Bachelor of Medicine/Bachelor of Surgery (MB, BS). He is a member of the Royal College of Physicians in London. He has extensive experience across Clinical Development and International Medical Affairs. His career in the pharmaceutical industry began when he joined Glaxo Group Research in Clinical Pharmacology.
Leadership Lessons
“Probably the most important leadership experience came in my early career, when I became a Medical Director of a country – in that case Australia – where I had to operate with a greater degree of independence, lead quite a large team at the time, and balance all the diverse demands of the different stakeholders that interact with you: patients, physicians, researchers, regulators and internal colleagues in the business. I learned a great deal there about my leadership style: what my values were and what my drivers were, particularly through facing difficult issues and talking, reflecting on what we were trying to achieve; why and how you’re going to do that; and staying true to yourself in managing through those difficult topics.
“In terms of the sums, we had some financial challenges. I had to find a way of making my organization more efficient and responsive, and that was an important – and also, at the time – difficult experience. I then took on more senior global roles and an important step there (which I think applies to a lot of leaders in pharma and Medical Affairs) is managing globally dispersed teams with colleagues in lots of different time zones and countries. This involved balancing people with different cultural expectations, different perspectives on what good leadership looks like and how things should be communicated, how things should be managed, and managing and leading in that set-up.
“I’ve learned something from every leader I’ve had, in terms of how I’ve evolved and grown. In my leadership approach, one important learning I had with a leader was when one day I went to ask if I could do something and they said: ‘You should not be coming to ask my permission.
Come when you need my forgiveness.’ That was at a relatively early stage in my career and I think that gave me a perspective to take more personal responsibility and accountability for addressing situations and finding solutions. Not that it always went to plan, so I think then you accept you also have to take the responsibility for your decisions.
“Also, I had the privilege to work with leaders who modeled the best behaviors in terms of what ultimately is our priority in this industry, which is ensuring that the patients we serve receive the best treatments and optimum care and that we make sure that the trust they put in us as pharmaceutical healthcare companies is fulfilled. I would say that I learned equally from leaders who came from the commercial side of pharma and those who came from a scientific and medical side – all those different individuals have brought aspects to how my style of leadership has evolved.
“You don’t need to be the friend of your leader but, it’s important that you respect and understand their roles and actions and that they understand what you’re doing and how you’re doing it and what your vision is, and how that fits with the overall bigger picture.”



 “The ubiquity of mobile devices now means that we have an opportunity through these digital technologies to improve health outcomes: through basic communication services, but also highly innovative services with regard to tracking and sensor development, measurement of biometrics and delivery of medical services.” He suggests that the vision for digital health is nevertheless relatively straightforward: “It’s not just about providing information, but rather providing integrated services that are proven to improve clinical outcomes.”
“The ubiquity of mobile devices now means that we have an opportunity through these digital technologies to improve health outcomes: through basic communication services, but also highly innovative services with regard to tracking and sensor development, measurement of biometrics and delivery of medical services.” He suggests that the vision for digital health is nevertheless relatively straightforward: “It’s not just about providing information, but rather providing integrated services that are proven to improve clinical outcomes.” Health technology companies, academia, HCPs, and patients – as well as pharmaceutical companies – are delivering these digital solutions successfully. Butler highlights a couple of examples, including GlycoLeap’s diabetes system. “This tracks the obvious things like your activity, your nutrition, your glucose levels and your body mass index, but also combines it with a behavioral psychologist and nutritionist that you can access at any time. Basically, you get a personalized diabetes management program through your smartphone app, which would never have been dreamed about 10 years ago.”
Health technology companies, academia, HCPs, and patients – as well as pharmaceutical companies – are delivering these digital solutions successfully. Butler highlights a couple of examples, including GlycoLeap’s diabetes system. “This tracks the obvious things like your activity, your nutrition, your glucose levels and your body mass index, but also combines it with a behavioral psychologist and nutritionist that you can access at any time. Basically, you get a personalized diabetes management program through your smartphone app, which would never have been dreamed about 10 years ago.” “The problem is that this ‘one-bucket’ perspective on digital means that the ‘commercial produce/medical review’ approach is extended into digital activities where it is not appropriate. Provision of digital health solutions is one such area. To me, these are health interventions that solve problems for patients and there is a very clear analogy with the health interventions we call medicines. We have a moral duty to protect patients using such interventions from harm, respect their autonomy and maximize the benefit they can gain.”
“The problem is that this ‘one-bucket’ perspective on digital means that the ‘commercial produce/medical review’ approach is extended into digital activities where it is not appropriate. Provision of digital health solutions is one such area. To me, these are health interventions that solve problems for patients and there is a very clear analogy with the health interventions we call medicines. We have a moral duty to protect patients using such interventions from harm, respect their autonomy and maximize the benefit they can gain.”

 For Anne Welsh, Executive Coach and founder of Synthesis-in-the-City, the first step for a leader is to have a willingness to be self-reflective and, from being self-reflective, to build greater self-awareness over time. “If we think about the old style of leadership, it was very different from now where leaders are asked to be a lot more relational. Personally, I think that it takes courage to build self-awareness, because if you become more self-aware in one area, if you like, you have to actually open to your shadow as well as the positive aspects of self-awareness. So, I think self-awareness is a leadership journey and it demands courage.”
For Anne Welsh, Executive Coach and founder of Synthesis-in-the-City, the first step for a leader is to have a willingness to be self-reflective and, from being self-reflective, to build greater self-awareness over time. “If we think about the old style of leadership, it was very different from now where leaders are asked to be a lot more relational. Personally, I think that it takes courage to build self-awareness, because if you become more self-aware in one area, if you like, you have to actually open to your shadow as well as the positive aspects of self-awareness. So, I think self-awareness is a leadership journey and it demands courage.”

 The amount of data we are currently generating is astronomical. According to one often-quoted article on Forbes.com, some 90 percent of the data in the world was generated over the past two years alone. [1]
The amount of data we are currently generating is astronomical. According to one often-quoted article on Forbes.com, some 90 percent of the data in the world was generated over the past two years alone. [1] “In Medical Affairs, we have a unique role because we have a deep understanding of our products and knowledge of diseases. We should be looking to fit the new knowledge and insights that we can collect from Real-World Evidence (RWE) into delivering even better solutions for patients and the healthcare system. And, because we are in daily contact with healthcare professionals, patient associations and other stakeholders, we should be the ones who play a critical role in transforming that into something that actually meets the needs and provides services and solutions for end-users. By connecting what’s coming out of our R&D, the strategy behind the products from a commercial point of view, we could build this into an overall, integrated patient care vision.”
“In Medical Affairs, we have a unique role because we have a deep understanding of our products and knowledge of diseases. We should be looking to fit the new knowledge and insights that we can collect from Real-World Evidence (RWE) into delivering even better solutions for patients and the healthcare system. And, because we are in daily contact with healthcare professionals, patient associations and other stakeholders, we should be the ones who play a critical role in transforming that into something that actually meets the needs and provides services and solutions for end-users. By connecting what’s coming out of our R&D, the strategy behind the products from a commercial point of view, we could build this into an overall, integrated patient care vision.” Dr Devoy sees scope for applying digital innovation across a range of areas but suggests that R&D, patient outcomes, and safety are the three to focus on initially. There is significant potential for how we conduct clinical trials: for example, using artificial intelligence (AI) within R&D as part of the drug discovery process, and also helping to better characterize and stratify disease and the according patient populations for study.
Dr Devoy sees scope for applying digital innovation across a range of areas but suggests that R&D, patient outcomes, and safety are the three to focus on initially. There is significant potential for how we conduct clinical trials: for example, using artificial intelligence (AI) within R&D as part of the drug discovery process, and also helping to better characterize and stratify disease and the according patient populations for study. “We read every day about how digital is transforming everything we do – be that personal finance, or interactions with retail – so I think the expectation from society is that healthcare will also transform in that way. But, clearly, healthcare has quite rightly some additional challenges relating to the sensitivity of people’s health data and taking the right care of that. So, we need to work with regulators, governments, patients and physicians to make sure that these solutions are accessible, trusted, compliant and fitted to people’s expectations.
“We read every day about how digital is transforming everything we do – be that personal finance, or interactions with retail – so I think the expectation from society is that healthcare will also transform in that way. But, clearly, healthcare has quite rightly some additional challenges relating to the sensitivity of people’s health data and taking the right care of that. So, we need to work with regulators, governments, patients and physicians to make sure that these solutions are accessible, trusted, compliant and fitted to people’s expectations. “One thing I believe we’ve done very successfully is build up an approach for actively seeking external collaboration. ”Among the initiatives is a global program called Grants4Apps, established in 2013, where Bayer reaches out to companies that are in the early stages of developing in the digital health and care space. Bayer acts as incubator and offers mentoring support and access to Bayer expertise and knowledge to help them develop their business models and solutions. Meanwhile, the Grants4Apps Dealmaker program is a unique opportunity to acquire Bayer as a customer and is tailored for mature teams, startups and companies that have a solution ready to go for identified challenges.
“One thing I believe we’ve done very successfully is build up an approach for actively seeking external collaboration. ”Among the initiatives is a global program called Grants4Apps, established in 2013, where Bayer reaches out to companies that are in the early stages of developing in the digital health and care space. Bayer acts as incubator and offers mentoring support and access to Bayer expertise and knowledge to help them develop their business models and solutions. Meanwhile, the Grants4Apps Dealmaker program is a unique opportunity to acquire Bayer as a customer and is tailored for mature teams, startups and companies that have a solution ready to go for identified challenges.