The insights and perspectives presented in this article were informed by discussions held during a MAPS AMERICAS Roundtable meeting. We extend our sincere gratitude to all participants whose thoughtful contributions and candid sharing of experiences have enriched this content.
The influence-engagement disconnect in modern healthcare
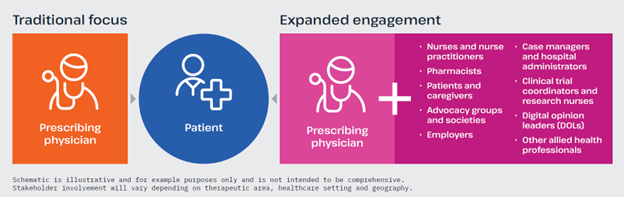
The healthcare landscape has evolved dramatically over recent years, with patient care increasingly dependent on a diverse network of healthcare professionals (HCPs) beyond the prescribing physician. While traditional Medical Affairs engagement has primarily focused on “typical” prescribers, this approach often creates blind spots that limit impact across the patient journey. Today’s reality is that while they may not all write prescriptions, multiple stakeholders strongly influence treatment decisions, patient education and ultimately patient outcomes. As treatment pathways grow more complex and patient-centred care becomes the standard, pharmaceutical companies must reevaluate who they engage with and how they deliver scientific information to the appropriate stakeholder at the right point along the patient journey. Below, we outline the critical contributions of a broader group of stakeholders (see Figure 1) and present actionable strategies for Medical Affairs teams to build meaningful, impactful engagement.
Figure 1. The evolution from traditional physician-focused engagement towards broadening Medical Affairs stakeholder engagement.
Key stakeholders beyond the prescribing physician
Nurses and advanced nurse practitioners
Nurses and advanced nurse practitioners represent one of the most influential yet often under-engaged stakeholder groups. As frontline providers, they frequently have more direct patient contact than physicians and often across a longer period, making them crucial for education and treatment support.
In many therapeutic areas, especially in chronic conditions and oncology, nurses serve as the primary point of contact for patients navigating complex treatment regimens. They are required to translate complex medical information into practical guidance and often facilitate difficult conversations about treatment expectations. Advanced nurse practitioners have increasingly expanded roles, particularly in community settings, that include prescribing and greater involvement in treatment decisions. A Sermo survey of 241 nurse practitioners in the United States found that 29% were actively involved in treatment decision making, with 20% also indicating they played a role in diagnosis.1 Ensuring that this key group has access to the same breadth of scientific information as physicians is not just beneficial—it’s essential for optimal patient care.
Pharmacists
Pharmacists are medication experts whose influence extends far beyond dispensing alone; their expertise in pharmacology, drug-drug interactions and administration protocols make them essential partners in ensuring safe and effective patient management.
Hospital and specialty pharmacists are increasingly integrated into multidisciplinary care teams, where they provide real-time consultation on complex medication regimens and actively participate in treatment planning. Additionally, their involvement in guideline development and formulary decisions directly impacts treatment access.
For many patients, community pharmacists are the most accessible HCPs. They play a critical role in identifying adherence challenges, managing side effects and coordinating with other providers to optimise therapy. As pharmacy services continue to expand, pharmacists are assuming greater responsibility for patient education and ongoing monitoring, particularly for high-cost, complex therapies.
Patients and caregivers
The patient voice has, quite rightly, gained prominence as patients and caregivers evolve as active partners in healthcare decision making. This important shift towards patient-centred care emphasises why we must better understand the needs, preferences and challenges these stakeholders face. As healthcare becomes more personalised and complex, patients and their caregivers require access to clear, accurate information to enable them to participate meaningfully in shared decision-making processes.
In paediatric and elderly populations, where caregivers often serve as primary decision makers and treatment administrators, effective and timely communication becomes even more critical. Family members managing care for children or aging parents need support to navigate and monitor treatment regimens and communicate important observations back to HCPs. Their firsthand experiences provide invaluable insights that cannot be captured through provider interactions alone. For many conditions, particularly chronic and rare diseases, these patient voices hold collective knowledge that matches that of many specialist HCPs.
Advocacy groups and societies
Patient advocacy groups and societies serve as the collective voice of patients and caregivers across the healthcare landscape. As knowledgeable partners, they have significant influence in shaping treatment guidelines, healthcare policy, research priorities and educational initiatives that directly impact how care is delivered. These organisations frequently function as gatekeepers to broader professional communities through their conferences, publications and continuing education programmes, offering efficient channels to reach specialised HCPs who may otherwise be difficult to engage individually. As a crucial bridge between industry, HCPs, and patients, these groups are uniquely positioned to facilitate the multidirectional communication and collaboration necessary to accelerate innovation and improve patient outcomes.
Other under-engaged stakeholder groups
Several other stakeholder groups are gaining prominence and deserve consideration in comprehensive engagement strategies, each offering unique value and perspective.
Employers increasingly influence healthcare decisions through benefits design, wellness programmes, and direct contracting with providers. As they take more active roles in managing employee health costs and outcomes, they require scientific information to inform coverage decisions.
Case managers and hospital administrators play crucial roles in determining treatment pathways and access. Their focus on care coordination, resource utilisation and system efficiency significantly impacts which treatments are readily available and how they are delivered to patients.
Clinical trial coordinators and research nurses directly influence study recruitment, protocol adherence and patient retention. Their frontline experience provides valuable insights into protocol feasibility, patient burden, and potential barriers to trial participation.
Digital opinion leaders (DOLs) represent a newer but rapidly growing influence category, leveraging social media, podcasts, blogs, and other digital platforms to share scientific perspectives that reach far beyond traditional academic channels.
Other allied health professionals, including pathologists, psychiatrists, psychologists, physician associates, physiotherapists, respiratory therapists and nutritionists, also play critical roles in treatment implementation and/or ongoing patient support, particularly in chronic conditions where multidisciplinary care is essential.
Challenges in engaging nonprescribing stakeholders
Time and access constraints: Finding windows of opportunity
Not unexpectedly, engaging with diverse stakeholders can present significant logistical challenges for Medical Affairs teams. Reaching a broader network frequently requires navigating unfamiliar institutional protocols or departmental structures, and nonprescribing HCPs often operate under different time constraints and within distinct practice settings. For example, hospital nurses often work in highly structured environments with minimal flexibility for additional education or industry interactions. They likely have limited or no internet access during working hours, and creative approaches to engagement may be required.
Creating targeted content to meet diverse audience needs
Developing content appropriate for different stakeholders represents another significant challenge in broadening engagement. Each group has unique information needs, has preferred formats and channels, and requires different levels of scientific detail tailored to their specific role in patient care. For example, materials designed for physicians often fail to address the practical implementation questions that nurses, pharmacists, and other stakeholders encounter in daily practice. They also rarely provide content suitable for these stakeholders to use with their patients. A recent Sermo survey of nurse practitioners in the United States found that e-learning courses, case studies and video presentations were their most preferred content formats,1 illustrating the importance of understanding these specific preferences when developing materials.
“Materials designed for physicians often fail to address the practical implementation questions that nurses, pharmacists, and other stakeholders encounter in daily practice.”
While scientific rigor must be maintained, information must be adapted to suit different contexts and applications. This requires understanding the distinct needs, decision points and knowledge gaps for each audience, which often means gathering insights that are not readily available within a pharmaceutical organisation that may have traditionally concentrated on prescriber needs. The challenge extends beyond content development to engaging through preferred communication channels. Different stakeholder groups may be active on different platforms, from specialised professional forums like the Hematology/Oncology Pharmacy Association (HOPA) forum for oncology pharmacists, to region-specific social networks or messaging applications. Such channel-specific engagement strategies often require collaboration across medical, legal, regulatory and digital teams to ensure they are effective and compliant.
“While scientific rigor must be maintained, information must be adapted to suit different contexts and applications. This requires understanding the distinct needs, decision points, and knowledge gaps for each audience, which often means gathering insights that aren’t readily available within a pharmaceutical organisation that may have traditionally concentrated on prescriber needs.”
Resource prioritisation
Perhaps the biggest practical challenge is determining how to allocate limited Medical Affairs resources across an expanded stakeholder landscape. With finite budgets and personnel, teams must make strategic decisions about which stakeholder groups to prioritise, when to engage them and what level of investment to make. These decisions demand careful consideration of potential impact, therapeutic area needs, organisational capabilities, and alignment with broader medical strategy. This challenge is particularly acute in smaller companies where engagement decisions can feel reactive rather than part of a considered systematic approach. There are currently mixed capabilities when it comes to demonstrating return on investment by measuring the value of engaging nonprescribing stakeholders, which can make resource allocation decisions particularly challenging.
Opportunities for strategic engagement
Understanding stakeholder needs at different points in the patient journey
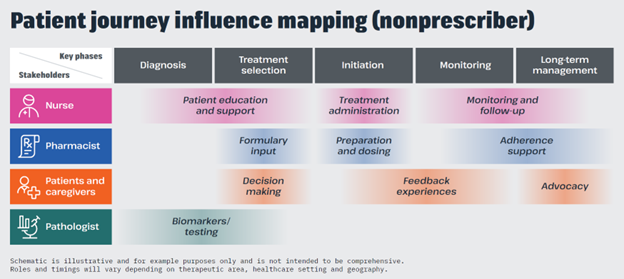
Effective engagement with nonprescribing stakeholders begins with mapping their specific roles, information needs and influence points throughout the patient journey. This journey-based approach helps identify where and when stakeholders have the greatest impact on patient outcomes, revealing natural opportunities for targeted, meaningful engagement and helping guide decisions on where resources are best allocated. I have seen firsthand how organisations that invest time in this journey-mapping exercise consistently identify engagement opportunities they had not previously considered, often in areas where their competitors have yet to establish a presence. Importantly, which stakeholder groups play the most significant roles, and when, also varies across therapeutic areas, healthcare settings and geographies, making this journey-mapping exercise essential for each specific context (see Figure 2).
“[A patient] journey-based approach helps identify where and when stakeholders have the greatest impact on patient outcomes, revealing natural opportunities for targeted, meaningful engagement and helping guide decisions on where resources are best allocated.”
Figure 2. Nonprescribing stakeholders play distinct roles across the patient journey. A comprehensive journey-mapping approach enables Medical Affairs teams to identify strategic engagement opportunities that best suit the needs of their target audience.
For a chronic condition, a nurse may interact with the patient more frequently than the physician, particularly during treatment initiation, when patients require education and support to navigate new therapies. Pharmacists may have greatest influence during treatment selection and monitoring phases, while patient advocacy groups typically become most important during diagnosis and at major treatment decision points. By understanding all these inflection points, Medical Affairs teams can deliver timely, relevant scientific information aligned to the needs of various stakeholders when they are most receptive and positioned to apply it.
Building relationships through specialty-focused engagement
Medical Affairs teams are increasingly recognising the value of engaging with specialty-specific organisations beyond participation in major medical congresses. This targeted approach allows for more relevant engagement with nonprescribing stakeholders in environments where they are actively seeking education and networking opportunities. For engaging with nurses, this might mean attending nursing-focused conferences or, more importantly, fostering ongoing relationships with larger professional associations such as the Oncology Nursing Society (ONS) or regional/local nursing societies. Parallel opportunities exist with pharmacy societies or patient advocacy groups, which can lead to collaborative research projects or the development of resources relevant to their members. Developing strong partnerships with specialty-specific organisations can open doors to more sustained and meaningful collaboration. These relationships enable Medical Affairs to co-create tailored educational programmes, support guideline development or participate in advisory boards focused on practical implementation of therapies. Importantly, these relationships also build the trust that underpins effective stakeholder engagement.
A comprehensive engagement strategy should include mapping not just where your target audience is likely to be and understanding their specific educational needs, but also which organisations they rely on for professional development and support. In my experience, organisations often overlook the value of these specialty-focused collaborations, yet they frequently offer more meaningful engagement opportunities than traditional physician-dominated activities.
Identifying and engaging DOLs
While DOLs represent an emerging area of focus, pharma companies are at different stages of developing strategies to engage with these influential voices. Some organisations are creating dedicated roles focused on digital engagement, while others are still working to overcome compliance barriers in this space. Digital forums can serve as valuable listening spaces and provide early insights into real-world challenges with new products. Active online DOLs may include familiar expert physicians but often extend to nonphysician experts such as nurses, pharmacists, patients, caregivers and patient advocates. Establishing best practices for partnering and co-creating content with this diverse group of influencers helps ensure credibility, reach and alignment with your organisation’s desired attributes and values.
Supporting early-career HCPs through targeted educational initiatives
Developing specialised educational resources for early-career HCPs can build valuable long-term relationships because these professionals often have different information needs than established KOLs. Specialty-specific organisations can be particularly effective partners for these initiatives, given their focus on professional development for newer practitioners. Effective approaches include developing mobile applications designed specifically for early-career professionals, creating mentorship opportunities and ensuring educational materials address fundamental questions that might be overlooked in materials targeting more experienced practitioners.
Measuring impact and value
As Medical Affairs teams expand their engagement beyond traditional prescribers, developing appropriate and specific measurements of success becomes essential. The contextualisation of those measurements, with outside factors such as landscape dynamics, leads to better evaluation of the impact of the work, the value that can be derived from it, and hence the security of continued resource investment. The most valuable measurements link engagement efforts to changes in belief and behaviour that lead to tangible healthcare improvements, whether through optimised treatment implementation, increased adherence, or improved patient experience. Although establishing these connections requires thoughtful measurement frameworks, something that we have focused on developing at HCG,2 demonstrating this broader impact provides compelling justification for comprehensive stakeholder engagement strategies.
Navigating the path forward
As the healthcare ecosystem continues to evolve, so too must our approach to Medical Affairs engagement. The insights shared throughout this article highlight several critical considerations for organisations seeking to maximise their impact across the full spectrum of healthcare stakeholders:
Nonprescribing stakeholders are essential to treatment success. While physicians remain important, the reality of modern healthcare delivery means that nurses, pharmacists, patients, caregivers and other stakeholders play pivotal roles in treatment decisions and outcomes. Their unique perspectives and influence points cannot be overlooked in comprehensive engagement strategies.
A patient-journey approach reveals optimal engagement opportunities. Mapping the specific roles and influence points of different stakeholders throughout the patient journey enables Medical Affairs teams to deliver the right information to the right audience at moments of maximum impact. This systematic approach also helps prioritise limited resources for greatest effect.
Early engagement drives better outcomes. Involving diverse stakeholders throughout the product lifecycle, from clinical development through postmarketing, creates opportunities to address practical implementation challenges before they arise. This proactive engagement requires planning and coordination yet ultimately supports better treatment experiences and patient outcomes.
Tailored, scientifically credible communication is key. While scientific rigor must be maintained across all stakeholder communications, information must be adapted to meet the specific needs and knowledge levels of each audience. One-size-fits-all approaches to scientific communication are increasingly ineffective in today’s specialised healthcare environment.
Measurement must evolve beyond traditional metrics. As stakeholder engagement expands, so too must our approach to measuring impact. Focusing on how engagement influences knowledge, behaviour and ultimately patient outcomes requires a deep understanding but provides more meaningful insights than traditional reach and frequency metrics.
By embracing these principles and developing thoughtful, comprehensive approaches to broader stakeholder engagement, Medical Affairs teams can position themselves as valued scientific partners across the healthcare ecosystem, ultimately supporting better decision making and improved patient care.
References
- Understanding today’s care team dynamics. Sermo Barometer Study #33; 17-23 April 2024. Available at: https://app.sermo.com/barometer (accessed July 2025).
- Quinn K and Bruce I, for HCG. Everyone wants impact — how do we start?; 12 June 2025. Available at: https://www.mmm-online.com/partnercontent/everyone-wants-impact-how-do-we-start/ (accessed July 2025).
About the author: Helen Langan is an Executive Vice President in the Medical Affairs division of HCG, a medical communications agency supporting pharmaceutical clients in strategic and tactical planning to meet the educational needs of their stakeholders. To find out more about how she can help you optimise your stakeholder engagement approach, reach out to her at [email protected]
INTERESTED IN HOSTING A ROUNDTABLE?
This article summarizes a Roundtable hosted by a MAPS Partner Circle member that brought together leading experts from across the industry. If you are a solution provider interested in hosting your own Roundtable, please check out our Media Planner or contact Luke with MAPS: [email protected].