Summary of MAPS New Orleans Roundtable hosted by Sermo on March 24, 2025
Roundtable Participants/Co-Authors
- Shivang Joshi, MD, MPH, RPh., FAHS, Neurology, Headache Medicine and Sermo Medical Advisory Board Member
- Zachary Horne, MD, Radiation Oncology and Sermo Medical Advisory Board Member
- Joanna Molke, VP, Marketing at Sermo
- Kaitlin O’Hara, Senior Director, Marketing at Sermo
Discussion Summary
As Medical education teams look to leverage new technologies and digital platforms, it’s critical to understand how physicians want to consume education. Drawing from their real-world experience as practicing physicians, Sermo Medical Advisory Board members Dr. Zachary Horne (Oncology) and Dr. Shivang Joshi (Neurology) provide practical insights on how to create more impactful and relevant communications for HCPs in a simple-to-implement “do THIS, not THAT” format.
Revolutionizing HCP Engagement: Key Insights from Sermo’s Roundtable
Sermo’s Roundtable discussion at MAPS offered an invaluable platform for Medical Affairs leaders to hear first-hand from HCPs as they share insights and practical strategies to enhance engagement in today’s evolving medical landscape. Guided by expert opinions and data-driven recommendations, participants gained actionable takeaways on improving interactions with physicians in an increasingly digital and personalized world. This article highlights 3 key insights from the “Do THIS, not THAT” discussion and how Medical Affairs professionals can apply them to maximize their impact.
1. Shifting Trends in Medical Congress Attendance
Do THIS: Prioritize sharing your medical congress and publication updates on-demand.
Not THAT: Assume physicians are all at the Congress!
In today’s complex and demanding healthcare landscape, it’s no longer enough to use traditional congresses as a primary channel to distribute new clinical data. In fact, Sermo’s research shows that roughly half of physicians only attend one to two medical congresses per year — yet they still need to stay informed on the latest advancements, publications, and standards of care.
Even when physicians do attend, they’re often forced to choose between multiple compelling sessions happening simultaneously. Dr. Joshi pointed out, the fear of missing out (FOMO) is real — and even among attendees, there’s a clear need for follow-up content. Dr. Horne echoed this sentiment, highlighting that retaining meaningful information often happens after the meeting, through formats that match individual learning preferences, such as reading concise summaries or reviewing curated content.
“The amount of meetings that I can actually go to is fairly limited just by the logistics of getting coverage in my own practice. Having access to live or pseudo-live updates from conferences is really high value.
When I go to conferences, I am there to network and hear the new releases but to retain anything, I need to read it later on so having access to insights from digestible sources is really helpful, I think social media is one of the best ways to get that information out there.” – Zachary Horne, MD, Radiation Oncology
On-demand access to congress highlights — through email digests, snackable infographics, and social media — helps bridge this gap. Physicians are looking for efficient ways to absorb critical updates amid packed clinical schedules. Centralized resources, curated “top 10” takeaways, and brief expert commentaries respect their time limitations while increasing the likelihood that the data will be understood, retained, and eventually applied in practice.
Organizations that invest in delivering content across channels — whether through open-access knowledge hubs, visually engaging summaries, or interactive social posts — are the ones truly meeting physicians where they are. As Dr. Horne noted, platforms that offer curated updates in real time, enriched with insights from key opinion leaders, are invaluable in keeping pace with today’s evolving standards of care.
2. The Power of Personalization in Medical Education
Do THIS: Personalize outreach based on physician preferences and practice needs.
Not THAT: Send generic, one-size-fits-all content.
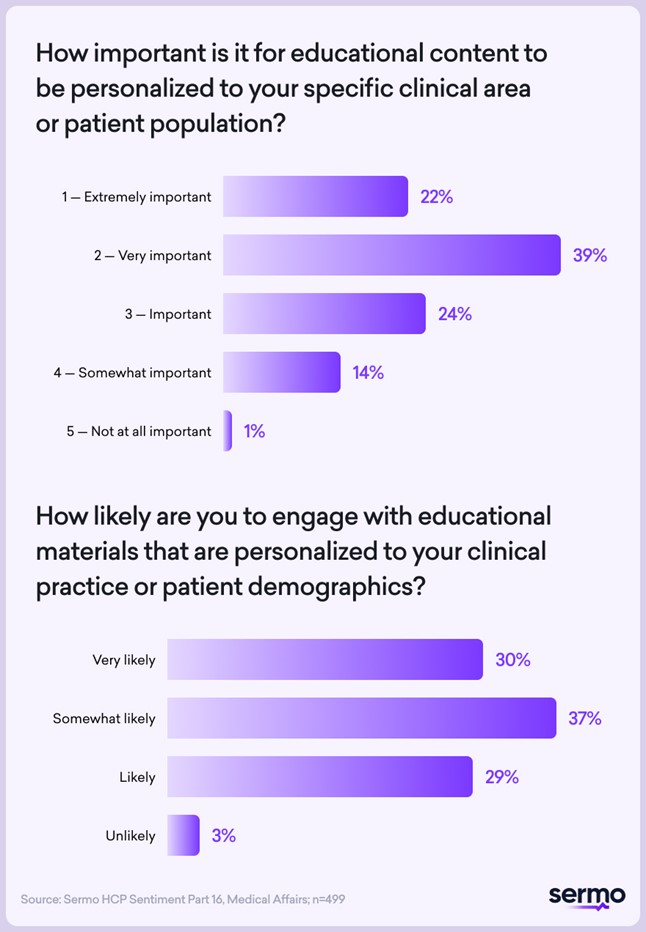
In an era of information overload, personalization has moved from being a “nice-to-have” to a non-negotiable. 61% of physicians say it’s extremely/very important that educational content is tailored to their specific clinical area or patient population. And the numbers don’t lie — 67% say they are very/somewhat likely to engage with content that is personalized to their clinical practice or patient demographics.
Dr. Horne brings this to life with a stark reality: hundreds of messages flood his workday — emails, team chats, staff alerts, patient inquiries — each one a potential ding or ring that contributes to stress, distraction, and ultimately, disengagement. Over time, even the sound of a notification can trigger a visceral reaction.
“On any given day, the number of emails, chats, and messages I receive that are just related to work could be in the hundreds. There are a lot of things that I blindly delete every day if they aren’t relevant to me! Having tailored content that is truly tailored to the physician you’re messaging is critical so that they will a) read it and b) not be alienated by the contact and not want further contact from you.” – Zachary Horne, MD, Radiation Oncology”
What cuts through the noise? Relevance. Physicians are deleting generic content without a second thought. Messages from unknown third-party Medical Affairs sources often feel disconnected from their actual practice and clinical needs — and those emails end up in the trash folder, or worse, create a negative company association.
The takeaway is clear: frequency should never outweigh relevance. Rather than bombarding HCPs with repetitive touchpoints, companies should focus on high-value, high-impact communications. If the content is meaningful, timely, and clearly aligned with a physician’s specialty and patient population, it’s far more likely to be opened, read, and appreciated.
In a world where attention is a precious resource, the organizations that take the time to get personal are the ones that stand out.
3. Authenticity in Content
Do THIS: Be real! Show HCPs true clinical applications.
Not THAT: Focus on simple cases that don’t reflect our experience in practice.
When it comes to engaging HCPs, real beats ideal — every time. One of the most consistent pieces of feedback from Sermo members is this: simplistic, textbook-style patient cases don’t reflect the messy, nuanced realities of clinical practice. HCPs want content that mirrors what they actually see in the clinic — patients with comorbid conditions, diagnostic ambiguity, and real-world challenges.
“What’s really been working in the field is case-based information. If you can fine-tune cases that are more real-world, including comorbid conditions, people relate to that more.” – Dr. Shivang Joshi, MD, MPH, RPh., FAHS, Neurology, Headache Medicine
The tip? Be real. Ditch the “cookie-cutter” cases and instead share scenarios that incorporate complexity. A migraine case becomes far more engaging when the patient also has anxiety or is navigating perimenopause — real-world layers that spark meaningful dialogue and reflection.
Medical Affairs teams are uniquely positioned to lead the charge here. By facilitating MSL-hosted roundtables, collaborating with physicians to share anonymized real cases, and focusing on nuanced risk stratification and disease-state education, they’re able to bring richer, more clinically relevant content to the table. These small-group case discussions — sometimes over dinner — drive deeper connection, trust, and learning.
And it’s not just theory. One example shared was a series of ADPKD-focused events where radiologists were brought in to interpret real patient imaging. These sessions were not only compliant, but widely praised for their realism and educational value. Another team used a case simulator app to walk providers through complex patients with overlapping conditions.
Equally important is matching the content to the provider’s level of expertise. The conversation with a general practitioner should differ from that with a specialist. Personalization of not just the content, but the depth, is crucial for resonance.
For companies unsure about compliance, there are creative workarounds. One approach is the sponsorship model: Medical Affairs teams partner with experts who develop educational case content independently, sidestepping promotional concerns while retaining authenticity. Another is leveraging post-marketing data and real-world evidence, which MSLs are well within their rights to discuss.
The bottom line? HCPs don’t want polished—they want real. They want complexity, context, and content that helps them navigate the challenges they face every day. And they want to hear it from people like them — peers, specialists, real-world clinicians.
A Future-Forward Approach to HCP Engagement
The insights shared during the Sermo Roundtable reinforce a critical truth: HCP engagement must evolve alongside the medical industry. From embracing personalized outreach to fostering more meaningful education, the future lies in meeting physicians where they are—both literally and figuratively.
Sermo remains committed to empowering HCPs and the broader medical community through actionable insights, innovative tools, and ongoing dialogue. By implementing these key takeaways, organizations can strengthen their relationships with HCPs and contribute to a more informed, engaged, and effective healthcare landscape.
To uncover all the “do THIS, not THAT” tips, download Sermo’s full HCP Sentiment Part 16 report at: https://www.sermo.com/business/hcp-sentiment-study-series/ or email [email protected].
INTERESTED IN HOSTING A ROUNDTABLE?
This article summarizes a Roundtable hosted by a MAPS Partner Circle member that brought together leading experts from across the industry. If you are a solution provider interested in hosting your own Roundtable, please check out our Media Planner or contact Luke with MAPS: [email protected].